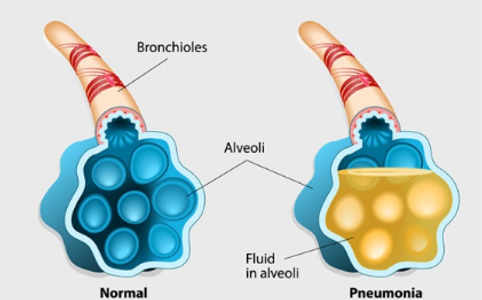
Pmeumonia is when the air sacs (alveoli) where the gas exchange takes place, become inflamed and filled with fluid and mucus, making it harder for you to breathe. The most common cause of pneumonia is by a bacterial infection – specifically a bacterium called streptococcus pneumoniae.
More people get pneumonia in winter. This is because other infections that spread easily from person to person, such as flu, are more common in the winter. Catching flu can increase your risk of developing pneumonia.
What are the numbers?
- 5-11 per 1,000 people in the UK get pneumonia each year.
- It is the 3rd greatest cause of death from lung disease after lung cancer (1st) and COPD (2nd).
- It is responsible for more hospital admissions and bed days than any other lung disease in the UK.
- It results in 220,000 diagnoses and 29,000 deaths per year.
Who is at risk?
- babies and young children
- people over 65
- people with long-term heart, lung and kidney diseases, or diabetes
- people with cancer, especially those having chemotherapy
- people who smoke or drink alcohol to excess
- people on drugs that suppress the immune system
As the risk of pneumonia increases with age, and with an aging population in the UK, (it is estimated that 23% of the population will be over 65 by 2035 vs 17% in 2010) it’s important for us to think about steps to minimise the occurrence of the disease.
How is pneumonia diagnosed?
The symptoms of pneumonia can develop suddenly over 24 to 48 hours, or they may come on more slowly over several days. It may be that a diagnosis can be made by discussing your symptoms and conducting a chest examination. This examination will involve using a stethoscope to listen for crackling or rattling sounds in your chest and back.They may also listen to your chest by tapping it – this will indicate the presence of pneumonia because lungs that are filled with fluid produce a different sound from normal healthy lungs.
However, there may be additional tests required to confirm a diagnosis, such as:
- Chest x-ray
- Blood test
- Sputum sample
What symptoms should you look out for?
There are a number of symptoms that may point to having pneumonia:
- a cough – which may be dry, or produce thick yellow, green, brown or blood-stained mucus (phlegm)
- difficulty breathing – your breathing may be rapid and shallow, and you may feel breathless, even when resting
- rapid heartbeat
- high temperature
- feeling generally unwell
- sweating and shivering
- loss of appetite
- chest pain – which gets worse when breathing or coughing
How is it treated?
- Antibiotics to treat the infection
- Chest physiotherapy
- Rest
- Painkillers for chest pain
- Some people may need to have IV antibiotics in hospital
The pneumococcal vaccine
One option to help protect yourself from pneumonia is to have the pneumococcal vaccine which encourage your body to produce antibodies against pneumococcal bacteria.
This is particularly important for the at risk groups. The types of vaccine and dosage frequency will depend on the age group:
- Babies receive 3 doses of pneumococcal conjugate vaccine (PCV) at 8 weeks,16 weeks and at 1 year. This vaccine is given to children up to the age of 2.
- People aged 65 and over only need a single pneumococcal polysaccharide vaccine (PPV).
- People with a long-term health condition may need just a single one-off pneumococcal polysaccharide vaccine (PPV) or vaccination every 5 years, depending on their underlying health problem.
- Children at risk of pneumococcal infections can have the PPV vaccine from the age of 2.
If you’re in any of the at risk groups we’ve mentioned don’t delay your pneumococcal vaccine – make an appointment with your GP today!